Abstract Authors
Lexia Henning - School of Molecular and Cell Biology, University of the Witwatersrand
Alfred Botha - Department of Microbiology, Stellenbosch University
Angela Botes - School of Molecular and Cell Biology, University of the Witwatersrand
Abstract Description
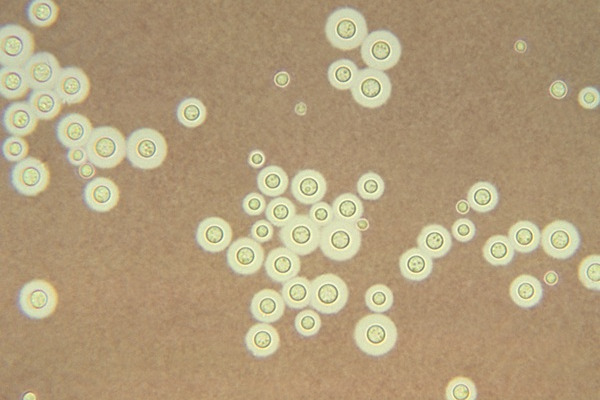
Antifungal drug resistance (AFR) poses a significant challenge in treating invasive fungal diseases (IFDs), particularly among immunocompromised individuals and those in resource-constrained settings such as South Africa. Mycoses caused by Cryptococcus species are of critical concern due to their prevalence, high mortality rates, diagnostic difficulty, limited treatment options and increasing AFR. This resistance is often driven by single-nucleotide polymorphisms (SNPs) located in genes associated with antifungal targets such as ERG11. This study aims to firstly identify AFR trends and resistance-inferring SNPs in clinical and environmental Cryptococcus isolates. Second, the functional impact of the SNPs will be assessed through computational protein modelling, molecular docking and dynamic simulations. Isolates were subjected to antifungal susceptibility testing against fluconazole (FLC) using minimum inhibitory concentration (MIC) and minimum fungicidal concentration (MFC) assays, followed by PCR amplification and sequencing of ERG3 and ERG11, SNP identification, SNP-AFR correlation, protein modelling of cryptococcal lanosterol 14α-demethylase (ERG11) variants, molecular docking and competitive dynamic simulations with FLC and the natural substrate, lanosterol. Environmental Cryptococcus isolates exhibited increased AFR compared to their clinical counterparts (p < 0.001). Additionally, temporal and geographical analyses revealed that older (pre-2010) and Western Cape isolates exhibited lower AFR rates compared to newer (2018 onwards; p < 0.001) and Gauteng (p < 0.001) isolates, respectively. Further, a multitude of known and novel SNPs in Cryptococcus ERG11 were identified, including South African-specific variants that alter the resultant protein structure and drug interaction, favouring an extreme drug-resistant phenotype (FLC-MIC > 64 µg/mL). Several mutations were identified in the transmembrane domain, all three substrate recognition sites, and the heme-binding motif. This was emphasised in the docking and dynamic simulations by the decreased FLC affinity and increased lanosterol affinity when compared to a susceptible model of lanosterol 14α-demethylase. However, the effects of single variants and other resistance mechanisms cannot be ignored; thus, further research is required. These findings underscore the urgent need for multifaceted approaches to researching AFR mechanisms and in antifungal stewardship, particularly in at-risk populations and settings.